We’re marking Digitober, a month-long festival that celebrates the work of Greater Manchester’s digital sector by showcasing some of the digital projects and services that benefit Stockport residents. Earlier this year, we introduced our Local Digital Fund Discovery project to improve hospital discharges to social care. This latest blog provides an update on progress.
We are nearing the end of our Department for Levelling Up, Housing & Communities (DLUHC) sponsored Discovery project. We set out to see if we can use data to help improve our understanding of patient/client flow, all to reduce the amount of time people spend in intermediate care beds, improving outcomes. Through the discovery we have explored if there is a problem that can be solved using a digital solution and we began development of a prototype.
What have we developed?
Following several workshops and conversations with colleagues in Stockport, Manchester and Oldham we focussed on intermediate care beds, aiming to provide more intelligence to better understand available capacity and patient/client flow. As part of this we looked to provide insight on reasons why a client’s status hasn’t changed, looking for common themes and to monitor trends to answer questions around bed capacity.
We took an agile, iterative approach, developing prototype forms in SharePoint to capture data from four intermediate bed locations in Stockport with a basic dashboard developed in Excel. Developing this “minimum viable product” quickly enabled us to determine if this information would be useful to colleagues to support their decision making. While the information did appear to be useful, we discovered that there was not enough granular detail on the reasons why a social care client’s status hadn’t changed in recent days.
We therefore re-visited the online forms, adding additional information to determine if the client’s status hadn’t changed for the following reasons:
- Client unwell
- Client in recovery
- Client involved in Active Therapy
- Requires continuing health care (CHC) involvement
- Requires social work
- Awaiting home of choice
- Awaiting equipment
- Requires mental health assessment
- Awaiting package of care
- Awaiting transport
- Awaiting medication
- Other reason
After making the changes we ran additional training sessions with Therapists, Therapy Leads, Discharge Coordinators, Ward Trackers and other colleagues involved in the process, explaining the new form and the benefits to capturing the new data.
As new data was available, we had to re-design the dashboard too. It still includes the summary information on capacity, length of stay and changes over time, but we now can drill down to reasons and see how they differ over time and by location. We can also drill down further, looking at the information for individual beds. This information is anonymised, so we only see the necessary information without being able to identify individuals.
We also received feedback that it would be helpful to report the latest figures throughout the day, so our BI Development colleagues developed a routine to load the data several times a day. The dashboard now automatically refreshes when new data appears.
Some of the intelligence we are capturing via the new process could be sourced from multiple health and social care systems and ideally the systems would talk to each other. However, it is difficult to pull this data together at speed and it is likely to take a great deal of effort and time to remedy this. One major benefit of the work we are doing now is we can test if this data is useful before we explore any system changes or linkages, reducing delay and potential wasted effort. The discovery project has helped us focus in on what we really need, breaking down the problem we are trying to solve.
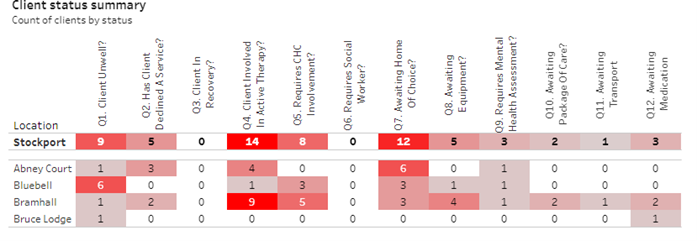
Table shows dummy data.
Next steps
We need to determine how scalable this solution could be, working with colleagues in Manchester and Oldham who are our partners for the Discovery. We are keen to work with the Greater Manchester Integrated Care System (GMICS) too, ideally looking to develop a solution that could be applied across Greater Manchester.
We also need to consider expanding the scope, potentially looking at other opportunities to connect data from both health and social care systems in a meaningful way. This would provide a longitudinal dataset to make it easier to plan and understand outcomes.

